Atrium Health Navicent Heart & Vascular Care
VATS - Video Assisted Thoracoscopic Surgery
What Is Video-Assisted Thoracoscopic Surgery?
Video-Assisted Thoracoscopic surgery is a minimally invasive surgical technique that allows a physician to diagnose a variety of problems involving the chest. These issues may include but are not limited to lung cancer, esophagus surgery, hiatal hernia, and lung surgery.
Video-Assisted Thoracoscopic surgery is an alternative to the most traditional thoracotomy, which involves the physical opening of the entire chest cavity, causing much trauma to the body, extending recovery times, and requiring more serious anesthesia and sedation of the patient, leading to further complications.
What Is the Procedure for Video-Assisted Thoracoscopic Surgery?
In contrast to the more heavy-handed thoracotomy, Video-Assisted Thoracoscopic surgery requires only tiny half-inch incisions, also called ports, through which small instruments can be introduced. This allows the physician to view the internal chest cavity on a screen.
Traditional thoracotomies require a single large incision between the patient's ribs through which the physician physically looks into. On top of being less precise, thoracotomies are also extremely uncomfortable, causing much pain and trauma to the patient.
VATS begins with general anesthesia, putting the patient to sleep so that he or she feels no pain. Anesthesia for VATS is usually administered through a mask, so patients will also require a tube down the throat for assisted breathing. This tube allows the patient to breathe through only one lung, so that the other can be completely deflated and allow the surgeon to view the chest cavity fully.
Occasionally, Video-Assisted Thoracoscopic surgery will be used to evaluate a problem inside the rib cage, usually in the musculature. In these cases, regional anesthesia is used instead. Patients will remain awake but feel no pain. This kind of anesthesia is administered via an injection in the back or neck. Even though the lungs are not being viewed directly, one of them might still need to be deflated so that doctors can move freely in the chest cavity.
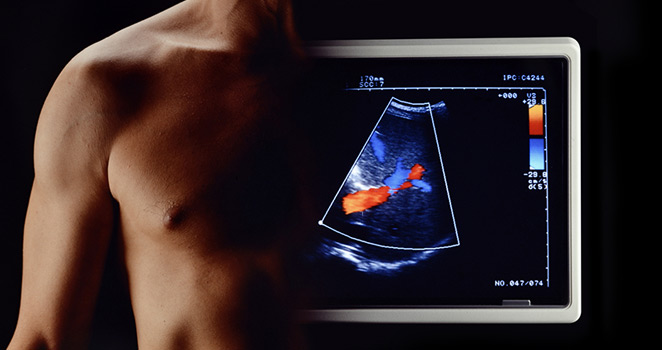
A small incision is made between the seventh and eighth ribs once the patient is satisfactorily sedated. Carbon dioxide gas flows into the chest through the opening so that the lung on that side deflates and collapses. Once this has happened, a thoracoscope, a camera attached to a flexible tube, is inserted through the incision. The surgeon can then view the image captured by this camera on video.
How Can I Prepare for Video-Assisted Thoracoscopic Surgery?
The first step to a successful Video-Assisted Thoracoscopic surgery is a consultation with your physician. He or she should answer your questions about the specific kinds of procedures that will be performed on you during your surgery and go into a bit of detail on each of them. It is also imperative that your physician tests for the pulmonary function to make sure you will recover well from the surgery.
In addition to pulmonary function, the following tests are also administered to measure overall health: blood tests, CT scan, and electrocardiogram. Some patients simply do not have the right profile of health, age, or lifestyle to undergo VATS.
It is also important to discuss the kinds of drugs you are taking and their dosages, especially if you are on insulin, which will interfere with medical tests. Blood thinners will most likely be stopped prior to the surgery as well, as they retard healing.
It is important to not eat or drink for eight hours prior to the procedure. An empty stomach ensures that the anesthesia will not cause nausea.
An anesthesiologist will go over your medical history and records the day of the procedure to discuss the best way to sedate you for the procedure.
How Long Is the Recovery Period after Video-Assisted Thoracoscopic Surgery?
The recovery time for VATS is relatively short compared to most surgical procedures.
Patients generally stay in the hospital for one day to recover from the surgery and anesthesia. Some will require a chest tube in the chest for a few days due to the buildup of fluid and the leaking of air.
If complications arise like fever, shortness of breath, or chest pain, patients may not be discharged for an even longer period of time.
A follow-up appointment is usually scheduled about a week after the surgery. At this time, the surgeon will look at the incision sites and assess your recovery. From his assessment, you will be given a clearer timeframe of when you can resume normal activities like work.
Complete recovery usually takes three to four weeks.
What Are the Risks of Video-Assisted Thoracoscopic Surgery?
Although Video-Assisted Thoracoscopic surgery is much less invasive with its traditional counterpart, there are still certain risks involved in any surgical procedure.
Though the incisions will be relatively small, they may leave unsightly scars on your chest.
Air leaks from the lung can occur, keep you in the hospital, and require additional treatment. In an extremely small segment of the population, significant bleeding can also occur.
All the risks that come with anesthesia will apply with Video-Assisted Thoracoscopic surgery.
The diaphragm and chest wall will be irritated for a few days or longer immediately following the surgery. The direct contact of the equipment on the inside of the chest cavity affects different patients in different ways, but generally, leaves a sense of discomfort for a while.
Post procedural fever is a common issue as well, occurring in 16% of patients.
Hemorrhage, lung perforation, and gas embolism are serious concerns, but happen in less than 1% of cases and are generally considered outlying cases.
Overall, VATS is much safer than thoracotomies because the incisions made are much smaller.