Atrium Health Navicent Heart & Vascular Care
Open Peripheral Vascular
What Is Peripheral Vascular Disease?
Peripheral Vascular Disease (PVD) is any number of diseases that occur in the blood vessels outside of the heart and the brain. Most common, is a narrowing of the blood vessels that carry blood to the extremities (legs, arms, etc.). Peripheral vascular disease comes in two forms: functional and organic.
Functional PVD does not have a distinct cause. Defects in the blood vessel's structure are undetectable and symptoms are temporary. Spasms in the blood vessels may occur and be triggered by temperature change, emotional distress, or smoking. One common example is Raynaud's disease. Functional PVD is generally not treated unless symptoms become more permanent and problematic.
Organic PVD is caused by structural damage to the blood vessels, usually by inflammation or tissue damage. Often, atherosclerosis or the buildup of plaque in the arteries is the root cause of organic peripheral vascular disease. Peripheral artery disease is a major example of organic PVD.
Symptoms of peripheral vascular disease depend on the artery affected and the severity of the blockage of blood flow. Dull pain, numbness, or tingling is common in patients who suffer from PVD.
Diagnosing peripheral vascular disease requires various testing and a physician needs to order an ultrasound Doppler, which allows him or her to look at the blood circulation in the arteries of the legs. A close look at the path of blood flow through the body helps the physician determine the kind of blockage a patient is suffering from, as well as the severity of the condition.
Once a diagnosis has been made, lifestyle changes must be made. Medication may be prescribed as well to manage the problem. In extreme cases, surgical procedures might be necessary.
What Is Open Peripheral Vascular Surgery?
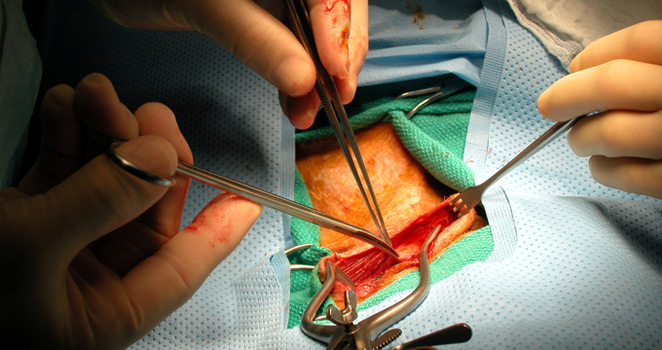
In extreme cases of artery blockage, it may be necessary to perform open surgery to correct the problem. Open peripheral vascular surgery tends to come in the form of a bypass for the blocked artery.
A bypass is formed when a surgeon around the blocked artery deliberately creates an alternative route for the blood. This detour can be created with a fabricated synthetic tube or harvested from a vein from the patient's own body.
A bypass is performed under anesthesia and may require large incisions. Because it is a major surgical procedure, physicians will exhaust all other options before resorting to open surgery.
What Are the Risks of Open Peripheral Vascular Surgery?
Because open peripheral vascular surgery is a relatively invasive procedure that requires anesthesia, it is subject to a number of risks and possible complications.
As with any other surgical procedure, infection is always a possibility. Because patients suffering from peripheral vascular disease are generally at risk for heart disease and heart attack, cardiac problems might arise during the procedure.
Furthermore, the large incisions necessary to perform the surgery take a long time to heal, and in some patients, never heal at all. Wounds that take long to heal require extended periods of rest and inactivity and may be prone to infection.
How Do I Avoid Open Peripheral Vascular Surgery?
Peripheral vascular disease is caused primarily by lifestyle choices that affect weight, blood cholesterol level, and blood pressure. Reducing all three of these will greatly reduce one's chances of being affected by PVD.
Managing one's weight through healthy eating and exercise is one of the most important decisions a patient suffering from PVD can make, even after open peripheral vascular surgery. Weight directly correlates with a higher risk of atherosclerosis and PVD.
Blood cholesterol level must be maintained and monitored for those at risk of heart disease. Once again, a healthy diet and regular exercise help to maintain the ratio of good and bad cholesterol.
Quitting smoking is the one lifestyle choice that may supersede all others. Across the board, smoking increases patient's risk for heart disease, elevated blood pressure, and heart attack.