Atrium Health Navicent Heart & Vascular Care
Artery Bypass Grafts Upper and Lower Extremities
What Is Peripheral Artery Disease?
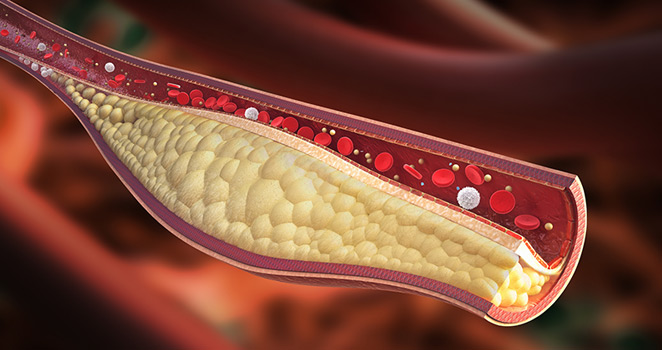
Patients who present with peripheral artery disease (PAD) generally suffer from a buildup of plaque in the arteries of the legs or arms. This buildup can be mild and require no treatment, but once the buildup of plaque is severe enough to cause blockages, they can cause pain and disable the patient. Walking can be impeded, and in advanced cases, patients can be at risk of losing the limb unless circulation is improved. Blood is necessary to transport oxygen and other vital chemicals throughout the body. Blockages prevent blood from traveling and "feeding" these limbs.
In cases where plaque buildup is extreme, a medical procedure might be required. Physicians tend to employ artery bypass grafts in upper and lower extremities to improve circulation and improve blood flow. This results in a reduction of pain, an increase in function ability, and an increase in the quality of life. Amputation is also prevented.
What Options Are Available to Treat Peripheral Artery Disease?
Patients who present with blocked peripheral arteries are generally given the option of stenting or angioplasty. These minimally invasive procedures are important ways to relieve a blockage so the patient can resume normal function quickly.
Angioplasty or stenting is a catheter-based procedure in which a catheter is inserted through a small incision, also referred to as an access point, and guided into the blocked artery. Using this catheter, a stent is guided into the artery to provide support for the damaged arterial wall. A balloon is slipped into the stent and inflated until the artery is the correct width, then deflated and removed. The stent is left in the artery. The surrounding tissue and cells grow around the stent, strengthening both the arterial walls and the stent itself.
While angioplasty is a good option for patients with simple cases of blockage, they tend to be much less durable and have major technical limitations when blockages are advanced. In these cases, artery bypass grafts for upper and lower extremities might be better options.
A primary care provider is best equipped, given an individual patient's medical history, age, lifestyle, and overall health to make a decision on which procedure is most appropriate. A history of vascular problems, prior treatments, the location and severity of the blockages are also key factors in whether or not a physician will recommend an artery bypass graft.
What Is an Artery Bypass Graft for Upper and Lower Extremities?
An artery bypass graft is a major surgical procedure that requires anesthesia. Because of its complexity and relative invasiveness as compared to angioplasty, it is not often the first choice made by a physician. Patients who are not good candidates for angioplasty or have already undergone angioplasty to poor results are often suitable for artery bypass grafts.
A surgical bypass treats a narrowed artery by creating a detour around the blockage of the artery. This detour is created by using a graft of a portion of one of the patient's own veins from another part of the body or a fabricated synthetic tube that can connect above and below a blockage. This allows blood to move through the detour, or bypass, rather than through the blockage itself.
What Are the Risks of an Artery Bypass Graft?
As with any major medical procedure, artery bypass grafts in the upper and lower extremities come with a host of risks.
Heart attacks, blood clots, and infections occur in 2 to 3 percent of patients who undergo the procedure. Because patients with advanced peripheral artery disease have a high frequency of heart disease and atherosclerosis, cardiac problems can be exacerbated by the procedure.
Medications that thin the blood like aspirin are necessary before and after the operation to reduce blood pressure. Blood pressure medications, as well as cholesterol-controlling drugs, are also commonly prescribed to patients undergoing artery bypass grafts.
The limbs themselves are also possible sources of major complications. Wounds incurred during the operation sometimes fail to heal. These wounds can be a considerable length because long incisions are necessary. Complications involving wound healing occur in roughly 1 in 5 patients, though these issues are easily managed with dressings or antibiotics.
Overall, artery bypass grafts for upper and lower extremities enjoy a 90-95% success rate. This success is highly correlated to the material used for the graft or the quality of the artery harvested as a detour.
What Is the Recovery Period Like After an Artery Bypass Graft?
The recovery time for an artery bypass graft depends on the surgical technique and skill of the surgeon. In general, patients can expect to stay in the hospital for fewer than 10 days. Staples and stitches from the incisions made are generally removed shortly after that, once a physician and deemed the wounds healed.
After discharge, assistance from a nurse, home aide, or physical therapist might be necessary in order to resume everyday activities. Most patients find they are able to recover fully and walk with less pain than before.
Your hospital stay may range from about 3 to 10 days. We will remove staples or stitches from the incisions, usually about 7 to 14 days after your operation after you leave the hospital. You may need assistance from a visiting nurse, home health aide, or physical therapist when you first go home.
A vein bypass in the leg can be expected to last over five years in 60 to 70% of patients, but about 1 in 4 patients will require follow-up procedures to maintain the function of their grafts.